Gallstone sludge is a common concern for many dealing with cirrhosis, prompting questions about effective treatments. Understanding the role of bile acids in this context is essential for health-conscious individuals. These compounds, particularly ursodeoxycholic acid, can help dissolve certain types of gallstones, improving liver health and patient comfort.
Cirrhosis often leads to a higher incidence of gallstones, making it critical to address this issue. Left untreated, gallstone sludge can contribute to severe complications, affecting quality of life. This guide will explore how bile acids can serve as a valuable solution, shedding light on their mechanisms and benefits.
Whether you’re looking for ways to manage your health or simply curious about the link between bile acids and gallstone sludge, this post aims to provide clear, practical insights. By understanding these connections, you can make informed choices that support your overall well-being.
Understanding Cirrhosis and Gallstone Formation
Cirrhosis significantly impacts the liver’s function and can lead to complications like gallstone formation. By exploring this connection, individuals can better understand how to manage their health, especially when considering the role of bile acids in gallstone sludge.
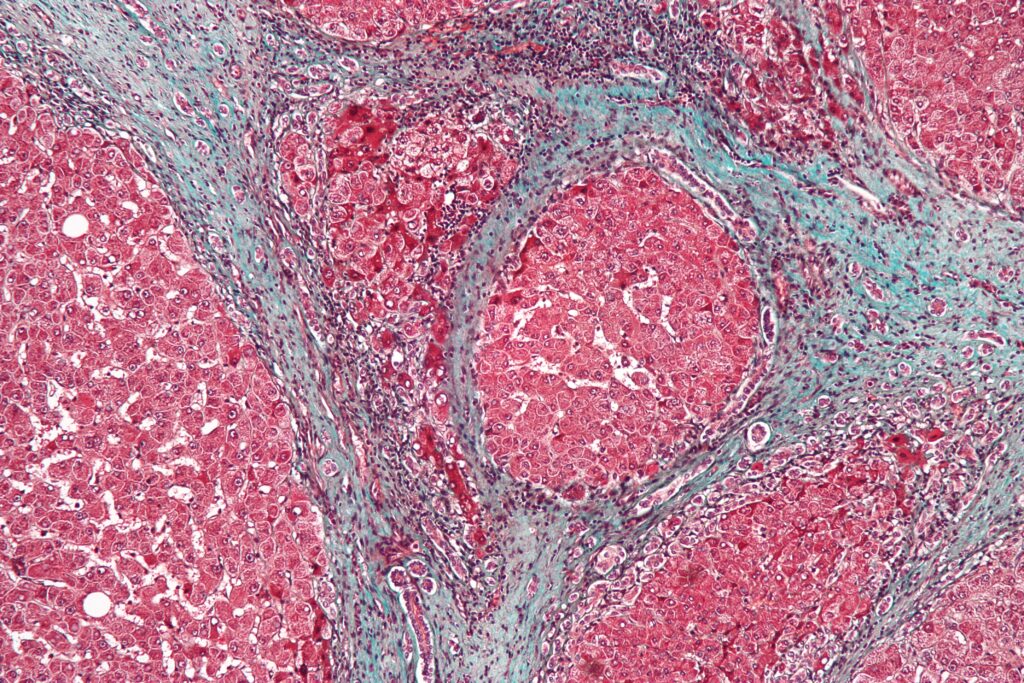
What is Cirrhosis?
Cirrhosis is a condition where the liver becomes scarred and damaged over time. This scarring disrupts normal liver functions, which can lead to serious health issues. Common causes of cirrhosis include:
- Chronic Alcoholism: Long-term excessive alcohol use can cause significant liver damage.
- Viral Hepatitis: Hepatitis B and C infections can lead to inflammation and scar tissue.
- Fatty Liver Disease: An accumulation of fat in the liver can result in cirrhosis, especially in individuals with obesity or diabetes.
Cirrhosis is often silent in its early stages, but as it progresses, it can lead to numerous complications including gallstone formation.
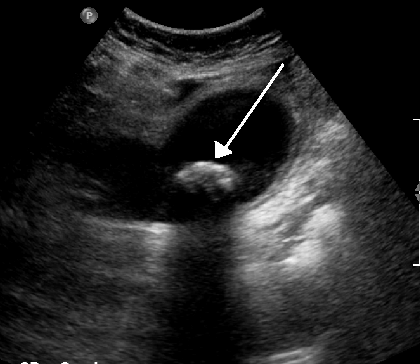
How Gallstones Form in Cirrhosis
Gallstones develop when the composition of bile, a digestive fluid produced by the liver, changes. In cirrhotic patients, the liver’s ability to effectively process bile can diminish. Here’s how this process unfolds:
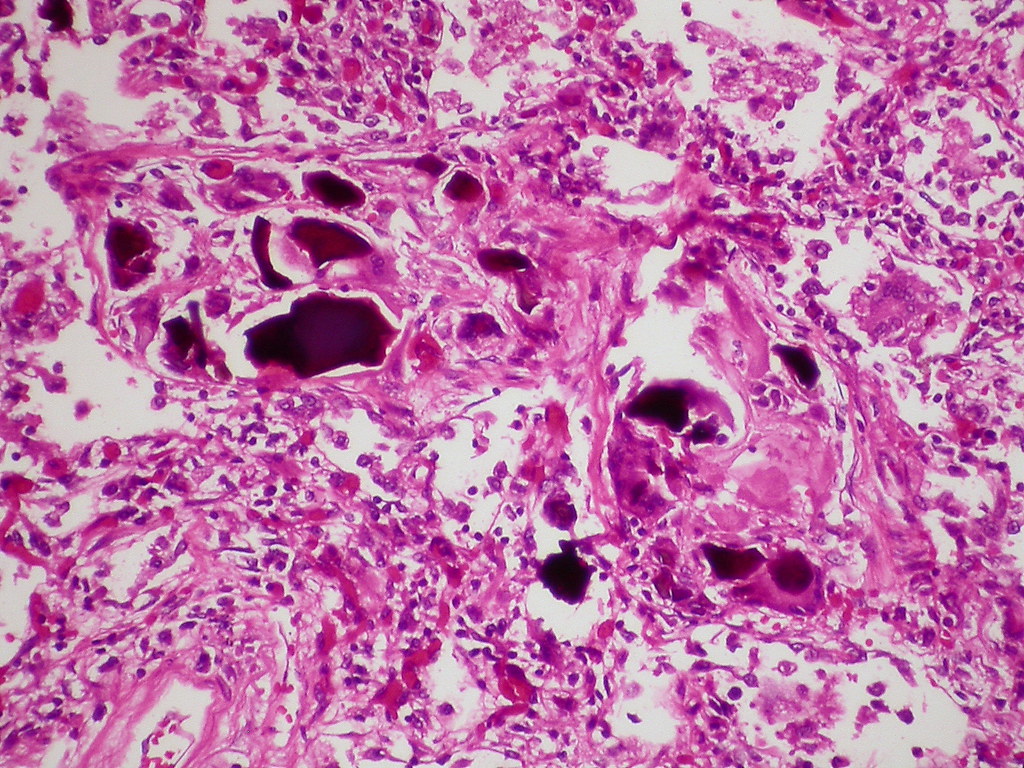
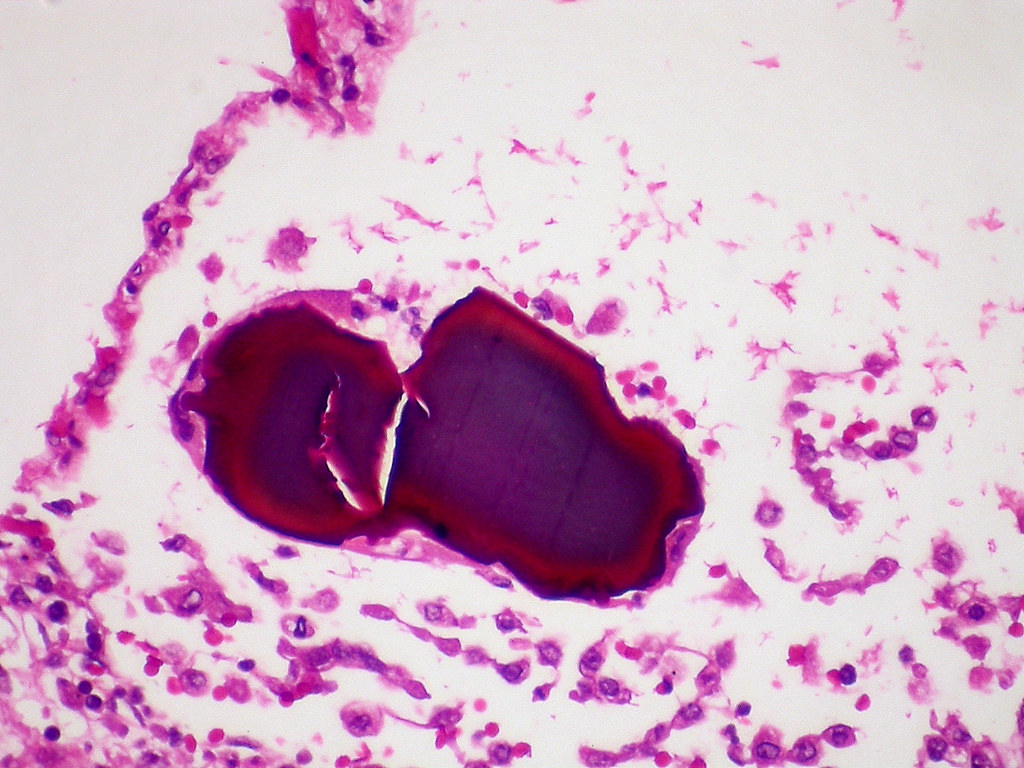
- Altered Bile Composition: Cirrhosis changes the balance of bile acids, cholesterol, and bilirubin in the bile. When the balance is disturbed, excess cholesterol or bilirubin can crystallize.
- Slowed Bile Flow: The scarring in the liver may impact the gallbladder’s ability to function optimally, leading to slowed bile flow. This stagnation encourages the formation of sludge and stones.
- Increased Risk Factors: Patients with significant liver disease tend to have higher cholesterol levels, further promoting gallstone development. The chronic liver condition can make gallstones more likely to form, especially in advanced stages.
Understanding these mechanisms can help in addressing treatment options such as bile acids for gallstone sludge in cirrhosis. For deeper insights, consider these resources: Gallstones in patients with liver cirrhosis, Gallstone Disease in Cirrhosis, and Close Relation Between Cirrhosis and Gallstones.
Role of Bile Acids in Treating Gallstone Sludge
Bile acids are crucial players in the management of gallstones, particularly for those affected by cirrhosis. Medications like ursodeoxycholic acid (UDCA) and chenodeoxycholic acid (CDCA) have shown promise in treating gallstone sludge. Understanding the types of bile acids and how they work can provide essential insights for anyone looking to improve their liver health.
Types of Bile Acids
There are two primary bile acids that are effective for treating gallstone sludge: Ursodeoxycholic Acid (UDCA) and Chenodeoxycholic Acid (CDCA). Each has unique properties that can aid in dissolution of gallstones.
- Ursodeoxycholic Acid (UDCA): This bile acid is one of the most well-studied for gallstone treatment. It works by decreasing cholesterol absorption from the intestines and reducing cholesterol secretion into bile. This action helps stabilize bile and is particularly effective in patients with cholesterol gallstones.
- Chenodeoxycholic Acid (CDCA): Similar to UDCA, CDCA also aids in dissolving cholesterol gallstones. It acts by altering the bile composition, leading to greater solubility of cholesterol. While it is effective, its use has diminished due to potential side effects compared to UDCA.
Both bile acids have been associated with various benefits, including:
- Reduction of gallstone size and quantity.
- Improvement of liver function in patients with cirrhosis.
- Potential relief from symptoms associated with gallstone sludge.
For more in-depth research on UDCA therapy and its impact on gallbladder disease, visit Ursodeoxycholic acid therapy in gallbladder disease.
Mechanism of Action
So, how do bile acids actually work to dissolve gallstones? The answer lies in their ability to modify bile composition and improve gallbladder function.
- Altered Bile Composition: Bile acids increase the concentration of bile salts, which play a vital role in emulsifying fats. This alteration allows for better mixing of cholesterol in bile, preventing it from crystallizing and forming stones.
- Enhanced Bile Flow: By stimulating the gallbladder to contract more effectively, bile acids help to flush out stagnant bile that may contribute to sludge and stone formation. This process essentially cleans up the bile, making it less likely for new stones to develop.
- Inhibition of Crystal Formation: Bile acids can decrease cholesterol saturation. When the bile is less saturated with cholesterol, the chances of crystal nucleation — the initial step in gallstone formation — are significantly reduced.
This knowledge highlights the importance of bile acids in managing gallstone sludge, especially in patients with cirrhosis. For a more detailed exploration of the effects of UDCA in gallstone dissolution, check out Gallstone Dissolution Effects of Combination Therapy with UDCA.
Bile acids offer a promising avenue for those looking to tackle gallstone sludge in the context of cirrhosis, making them a valuable component in treatment strategies.
Risks and Considerations
When exploring the use of bile acids for gallstone sludge in cirrhosis, it’s crucial to recognize the potential risks and considerations. While bile acids can offer therapeutic benefits, they may also come with side effects or might not be suitable for all patients. This section delves into these important aspects.
Side Effects of Bile Acids
Bile acid treatments can provide relief from gallstone sludge but can also lead to a range of side effects. Here are some common ones to be aware of:
- Diarrhea: This is perhaps the most frequent side effect. Bile acids increase bile flow, which can lead to loose stools.
- Nausea: Some patients may experience feelings of nausea, especially when starting treatment.
- Abdominal Discomfort: This includes cramping or bloating, which can occur as the body adjusts to increased bile acid levels.
- Skin Reactions: Some individuals might develop skin rashes or other allergic reactions.
- Altered Liver Function Tests: In rare cases, bile acid treatments could impact liver enzyme levels. Regular monitoring is advised to assess liver function during therapy.
Understanding these side effects can help you weigh whether the benefits outweigh the risks of bile acid therapy. Consulting with a healthcare professional is vital if you experience any troubling symptoms. For additional insights on managing side effects, consider visiting Management of Gallstones and Their Complications.
Who Should Avoid Bile Acid Treatment?
Not everyone is a candidate for bile acid therapy. Certain groups should proceed with caution or avoid this treatment altogether. These include:
- Patients with Severe Liver Disease: Individuals with decompensated liver cirrhosis may not tolerate bile acids well due to impaired liver function.
- Those with Gallbladder Obstruction: If there’s a blockage in the bile duct or gallbladder, bile acids may exacerbate complications.
- Pregnant Women: The effects of bile acids during pregnancy haven’t been adequately studied, making it safer to avoid them unless absolutely necessary.
- Allergic Reactions: Any known allergy to bile acids or related medications necessitates avoidance of such treatments.
- Certain Medical Conditions: Conditions like severe pancreatitis or intestinal diseases may contraindicate the use of bile acids.
By recognizing who should avoid bile acid treatment, patients can make informed decisions. Always consult with a healthcare provider to evaluate the risks tailored to your specific situation. For a deeper understanding of gallstones in the context of liver disease, further reading on Gallstones in patients with liver cirrhosis could be beneficial.
Lifestyle Changes to Prevent Gallstones
Making specific lifestyle changes can significantly reduce the risk of gallstones, especially for those with cirrhosis. Focusing on diet and regular check-ups can create a proactive approach to managing this condition.
Dietary Recommendations
What you eat plays a crucial role in gallstone prevention. Adopting a balanced diet can help manage bile composition, ultimately reducing the risk of stone formation. Here are some dietary tips to consider:
- Increase Fiber Intake: Eating foods rich in fiber supports digestion and bile health. Incorporate fruits, vegetables, and whole grains into your meals. At least five portions of fruits and vegetables daily can make a difference.
- Choose Healthy Fats: Include healthy sources of fat, such as olive oil, fish, and avocados. These can improve bile fluidity, aiding in gallstone prevention.
- Limit Refined Carbohydrates: Foods high in sugar and refined carbs can elevate cholesterol levels in bile. Cutting back on sweets, white bread, and sodas can be beneficial.
- Hydration is Key: Drinking adequate water helps in maintaining healthy bile production. Aim for at least eight glasses of water daily.
- Moderate Caloric Intake: Avoid crash diets or severely restricting calories, as this can increase the risk of gallstones. Instead, focus on consistent, balanced meals.
- Avoid High-Fat Foods: Heavy meals and foods high in saturated fats can contribute to gallstone formation. Limit red meats, processed snacks, and fried foods.
For comprehensive insights into dietary recommendations aimed at preventing gallstones, check out resources from the NIDDK and the NHS.
Importance of Regular Check-ups
Regular healthcare visits are essential, especially for those with a history of liver issues or gallstones. Why is monitoring so crucial?
- Early Detection: Regular check-ups can help detect changes in liver function or the formation of gallstones before they turn into serious complications. Early intervention often leads to better outcomes.
- Adjusting Treatment Plans: Ongoing care allows healthcare providers to tailor treatments based on individual progress. This continuous monitoring can help manage gallstone risks effectively.
- Professional Guidance: During check-ups, you can discuss dietary habits and lifestyle changes with your healthcare provider. They can offer specific advice based on your health status.
- Monitoring for Complications: Patients with cirrhosis are at higher risk for various complications, including gallstones. Regular health assessments help in promptly addressing any emerging concerns.
Staying proactive through regular check-ups can be the key to maintaining health and preventing complications. For more information on monitoring and preventive care, consider resources on regular health assessments and management strategies.
By making informed dietary choices and committing to regular healthcare visits, you can significantly reduce the risks associated with gallstone formation related to cirrhosis.
Emerging Research and Future Directions
Research into bile acids and their connection to gallstone sludge in cirrhosis is evolving, opening new doors for understanding and treatment strategies. The interplay between bile acids, the gut microbiome, and innovative therapies holds promise for improving patient outcomes.
The Gut Microbiome Connection
The gut microbiome is a complex ecosystem of microorganisms that live in our digestive tract. This community affects various bodily functions, including bile acid metabolism. But how exactly does it relate to gallstone formation?
- Bile Acid Regulation: The gut microbiome helps regulate bile acid composition. A balanced microbiome can convert primary bile acids into secondary bile acids, enhancing bile’s effectiveness in breaking down cholesterol. This process can potentially reduce the risk of gallstone formation.
- Metabolic Influence: An imbalance in gut bacteria can lead to altered bile acid profiles. This imbalance may increase cholesterol saturation in bile, a significant contributor to gallstone development. In cirrhosis patients, whose liver function is already compromised, these changes can exacerbate gallstone issues.
- Microbiome Interventions: Emerging studies suggest that probiotics or other microbiome-modulating therapies could play a role in managing gallstone sludge. By promoting a healthy gut flora, we might improve bile acid function and reduce gallstone risks.
This connection underscores the importance of gut health in managing cirrhosis and gallstone development. For further reading on the microbiome’s impact on health, consider exploring Bile acid metabolism and its relation to gut microbiota.
Future Therapies
The landscape for managing gallstone sludge through bile acids is evolving. New avenues of research and potential therapies are being explored, which could enhance treatment outcomes.
- Novel Bile Acid Therapies: Current research aims to develop new bile acids or combinations that may offer better efficacy with fewer side effects. Remarkable advancements are underway, especially with modified bile acids showing potential for superior solubilization of cholesterol.
- Combination Therapies: Integrating bile acids with other pharmacological agents could provide synergistic effects. For instance, pairing bile acids with gut microbiome modulators may enhance overall bile composition and reduce gallstone formation.
- Biomarker Developments: Identifying specific bile acids as biomarkers could help tailor treatments and predict gallstone formation risk in patients. Research suggests that certain bile acids might serve as metabolite biomarkers, guiding clinicians in personalized treatment approaches.
- Regenerative Medicine: Future therapies may also include using bile acids in liver regeneration strategies. By optimizing bile metabolism, we could potentially improve liver function and mitigate complications associated with cirrhosis.
The shift toward more personalized, multifaceted approaches in managing bile acids and gallstone sludge may revolutionize treatment strategies for cirrhosis patients. For insights on the latest research in bile acid therapies, explore Emerging role of bile acids as critical components in therapy.
Understanding these emerging connections and future directions is critical in shaping effective treatments and improving the quality of life for those affected by gallstone sludge in cirrhosis.
Conclusion
Understanding the role of bile acids in managing gallstone sludge for individuals with cirrhosis is crucial for enhancing liver health. Bile acids, particularly ursodeoxycholic acid, play a significant part in dissolving gallstones, ultimately improving well-being.
Taking proactive steps, such as discussing treatment options with healthcare providers, can empower patients to make informed choices about their health.
Engaging with this information may spark questions about how to integrate lifestyle changes or seek further research. Your journey toward better health starts with knowledge and awareness.

