Hypothyroidism is a common yet often overlooked issue in people with thalassemia, particularly those requiring regular blood transfusions. Studies show that thyroid problems can affect up to 30% of thalassemia patients, depending on the population and treatment standards. This connection is primarily linked to iron overload, which can damage the thyroid gland over time.
Early detection is key, as untreated hypothyroidism can worsen health conditions and hinder growth in children. Understanding the link between thalassemia and hypothyroidism can help ensure timely intervention and better outcomes.
What Is Thalassemia?
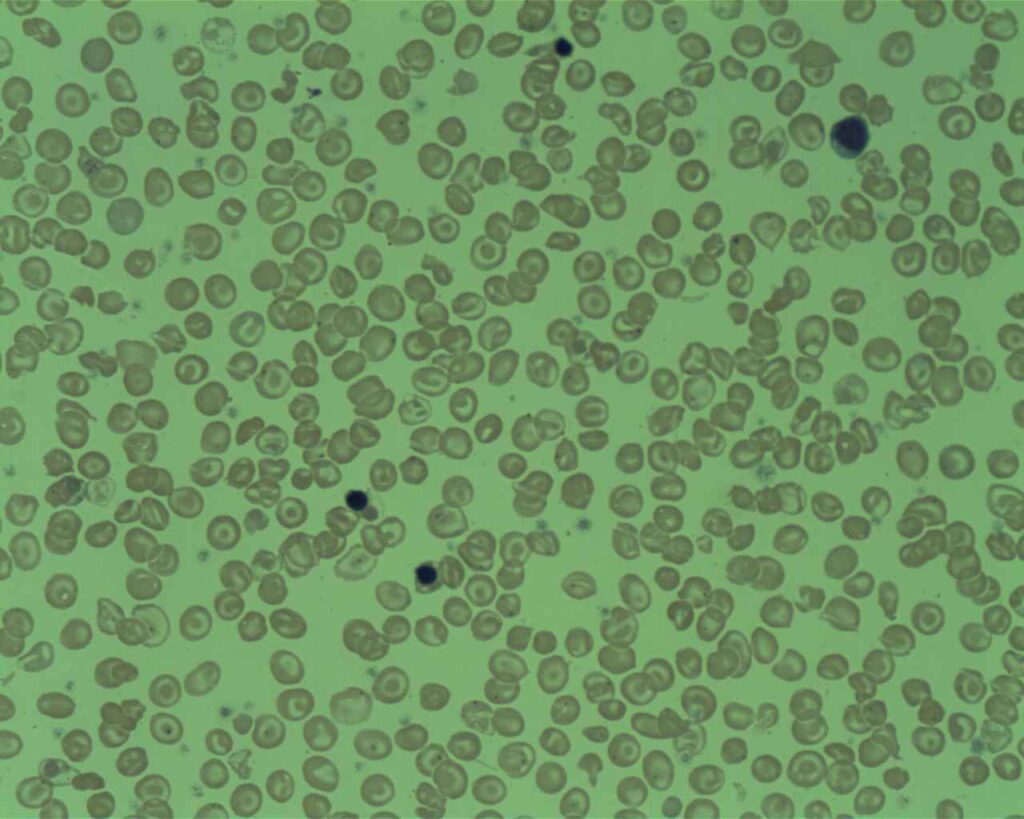
Thalassemia is a genetic disorder affecting the body’s ability to produce healthy red blood cells. For someone living with this condition, understanding its mechanisms can make everyday challenges less daunting. Let’s break it down so it’s easier to grasp.
How Thalassemia Affects the Body
At its core, thalassemia messes with hemoglobin, the protein in red blood cells responsible for carrying oxygen. When hemoglobin levels drop, the body struggles to transport oxygen effectively, leading to symptoms like fatigue or anemia. Thalassemia can range from mild to severe, depending on the specific genetic mutations a person inherits.
The condition stems from mutations in the genes responsible for hemoglobin production. There are two major types to be aware of:
- Alpha-Thalassemia: This type affects the alpha chains in hemoglobin, and its severity depends on the number of gene mutations involved.
- Beta-Thalassemia: This type involves the beta chains in hemoglobin and is often more severe, particularly in forms like beta-thalassemia major.
For more details on these types, visit Cleveland Clinic’s guide to thalassemias.
Signs and Symptoms You Should Know
Thalassemia often presents differently depending on its severity. Mild forms might cause little to no symptoms, while more severe cases can lead to a host of problems, including:
- Chronic fatigue: A constant lack of energy due to low oxygen levels.
- Pale skin and jaundice: Common in more severe thalassemia cases.
- Bone deformities: Especially in the face and skull due to bone marrow trying to compensate.
- Delayed growth in children: A result of chronic anemia or complications like hypothyroidism in thalassemia.
Symptoms can sneak up on you, making regular blood tests crucial to diagnosis.
How Is Thalassemia Diagnosed?
Doctors typically diagnose thalassemia through blood tests. A complete blood count (CBC) can reveal anemia, while additional tests like hemoglobin electrophoresis provide a deeper look at hemoglobin production. Genetic testing may be necessary for a definitive diagnosis, especially if family history points to the condition.
Early and accurate diagnosis is critical. Why? Knowing the type and severity of thalassemia helps tailor the best treatment plan, whether it’s regular blood transfusions, medications like iron chelators, or even bone marrow transplants in extreme cases.
For a comprehensive overview, check out Mayo Clinic’s resource on thalassemia.
Common Complications of Thalassemia
Thalassemia isn’t just about anemia; it can trigger a domino effect of other health issues. Chronic blood transfusions often lead to iron overload, damaging vital organs like the liver and heart. One lesser-known but significant complication is hypothyroidism, where the thyroid gland slows down. Studies have shown that iron buildup in thalassemia patients can harm the thyroid, causing symptoms like fatigue, weight gain, and feeling cold.
For insights on the relationship between thyroid dysfunction and iron overload, read this study on thyroid disorders in beta-thalassemia patients.
By understanding thalassemia better, you’re not only preparing for what’s ahead but also giving yourself—or a loved one—the tools to manage the condition more effectively.
What Is Hypothyroidism?
Hypothyroidism, also called an underactive thyroid, occurs when the thyroid—a butterfly-shaped gland in your neck—doesn’t produce enough hormones. It may seem small, but this gland plays a massive role in regulating metabolism, energy levels, and even temperature. When it slows down, nearly every system in the body can feel the impact. For people with thalassemia, this condition often develops as a secondary complication due to chronic iron overload affecting the thyroid.
Common Causes of Hypothyroidism
Hypothyroidism can happen for various reasons, but understanding the root cause is key to effective treatment. Here are the most common triggers:
- Autoimmune Diseases: Hashimoto’s thyroiditis is one of the main culprits. The immune system mistakenly attacks the thyroid, impairing its hormone production.
- Nutritional Deficiencies: A lack of iodine or selenium in the diet can slow down thyroid function.
- Medications and Treatments: Certain drugs or radiation therapy can damage the thyroid.
- Iron Overload: In conditions like thalassemia, excessive iron from regular blood transfusions can harm the thyroid gland.
For more details, visit Mayo Clinic’s overview on hypothyroidism.
Recognizing the Symptoms
Hypothyroidism often sneaks up on you with vague and mild symptoms, making it easy to overlook. Here’s what to watch for:
- Fatigue and sluggishness: A tell-tale sign caused by a slowing metabolism.
- Weight gain: Without changes in diet or activity levels, unexplained weight gain can indicate an issue.
- Cold sensitivity: Feeling chilly all the time, even in warm environments, could mean your thyroid isn’t working right.
- Constipation: Gut slowdowns are common when the thyroid gland underperforms.
- Puffy face and dry skin: These subtle signs often go unnoticed but are linked to fluid retention and slowed cell turnover.
Visit Cleveland Clinic’s guide on hypothyroidism symptoms for a deeper dive into more symptoms to look out for.
How Hypothyroidism Relates to Thalassemia
For individuals with thalassemia, hypothyroidism often results from iron deposits in the thyroid gland. Over time, the iron buildup can interfere with gland function, leading to hormone deficiencies. Studies suggest that 6-30% of thalassemia patients are affected by hypothyroidism, depending on age, transfusion frequency, and management of iron overload. More severe forms of thalassemia, like beta-thalassemia major, increase the likelihood of thyroid complications.
Learn more about the relationship between hypothyroidism and thalassemia in this research study on thyroid dysfunction in beta-thalassemia patients.
When it comes to managing your health, knowing the first signs of hypothyroidism can make a world of difference, especially for those managing thalassemia or similar chronic conditions.
The Connection Between Thalassemia and Hypothyroidism
Thalassemia, a genetic blood disorder, often involves a cascade of complications affecting various organs, including the thyroid gland. One such complication is hypothyroidism, which is intricately linked to the effects of iron overload and chronic hypoxia. Let’s explore these connections.
Iron Overload and Thyroid Function
In thalassemia patients, iron buildup is one of the leading causes of thyroid dysfunction. Frequent blood transfusions, a common treatment for severe thalassemia, can result in excess iron being deposited throughout the body, including the thyroid gland. Over time, this iron overload damages the delicate cells of the gland, impairing its ability to produce essential hormones.
The thyroid gland plays a critical role in regulating metabolism and energy levels. However, when iron infiltrates this gland, it disrupts normal function, leading to hypothyroidism. Studies consistently show that patients with thalassemia who experience poor iron chelation—meaning their body struggles to remove excess iron—are at a higher risk of developing thyroid problems. Read more on the correlation between iron overload and thyroid function.
Chronic Hypoxia’s Role
Chronic hypoxia, or low oxygen levels in the body tissues, is another significant contributor to hypothyroidism in thalassemia patients. As hemoglobin levels drop due to ineffective red blood cells, oxygen delivery throughout the body is compromised. This affects not only major organs but also glands like the thyroid.
Low oxygen availability leads to stress on the thyroid gland and other parts of the endocrine system. This condition exacerbates the risk of glandular dysfunction. Over time, the combination of hypoxia and iron overload creates a toxic environment that the thyroid simply cannot endure. Find out more about chronic hypoxia and endocrine health.
Subclinical vs Overt Hypothyroidism
Hypothyroidism presents itself in two primary forms: subclinical and overt. The distinction between the two is vital for understanding their prevalence and impact in thalassemia.
- Subclinical Hypothyroidism: This milder form involves elevated TSH (thyroid-stimulating hormone) levels, while T3 and T4 levels remain normal. Patients may feel fine and show no noticeable symptoms, but their thyroid is under stress and may progress to more serious issues.
- Overt Hypothyroidism: This form is more severe, with high TSH levels partnered with reduced levels of thyroid hormones (T3, T4). Symptoms like fatigue, weight gain, and cold intolerance are more pronounced.
Research suggests that subclinical hypothyroidism is more common in thalassemia patients; however, if left untreated, it can transition to overt hypothyroidism. Learn more about thyroid dysfunction in beta-thalassemia patients.
Understanding the delicate relationship between thalassemia, iron overload, chronic hypoxia, and hypothyroidism is essential for early intervention and tailored treatments.
Signs and Symptoms of Hypothyroidism in Thalassemia Patients
Understanding how hypothyroidism presents itself in those with thalassemia is crucial for early diagnosis and improved treatment outcomes. While thalassemia-related hypothyroidism shares many symptoms with typical hypothyroidism, the condition can also have unique aspects shaped by iron overload and chronic transfusions.
Early Warning Signs of Hypothyroidism
For thalassemia patients, hypothyroidism can creep in subtly with seemingly everyday symptoms. Paying attention to these early warning signs can make all the difference in catching the condition before it worsens:
- Unexplained fatigue: Feeling constantly drained, even after plenty of rest? This is a common red flag of a slowing metabolism.
- Cold sensitivity: Always reaching for a sweater, even when others feel fine? This intolerance to cold is another sign.
- Weight changes: Gaining weight without any major shifts in diet or activity levels suggests something could be off.
- Dryness and puffiness: Dry, flaky skin paired with a puffy face may indicate hormone imbalances.
- Digestive discomfort: Constipation and bloating are signs the body’s processes are slowing down.
Hypothyroidism doesn’t always announce itself loudly. Some symptoms, such as fatigue or skin changes, can seem too minor to worry about, but they’re worth flagging to your doctor.
Symptoms Specific to Thalassemia Patients
Due to chronic blood transfusions and iron overload in thalassemia, symptoms of hypothyroidism may overlap with or amplify existing health challenges these patients face:
- Growth delays in children: Hypothyroidism can stunt growth in thalassemia patients, compounding the developmental delays already tied to the condition.
- Delayed puberty: Low thyroid activity can throw off the hormonal balance needed for normal puberty.
- Short stature: This symptom is often linked to untreated hypothyroidism in young thalassemia patients.
The prevalence of these symptoms makes it clear why regular hormonal testing is crucial for children and adolescents with thalassemia.
Signs of Advanced Hypothyroidism
If hypothyroidism goes unnoticed or untreated, symptoms can worsen, leading to more serious complications:
- Hair thinning or loss: Hair becomes brittle, breaking easily, or starts to thin.
- Hoarseness: A slow thyroid can affect the vocal cords, causing a change in voice.
- Muscle weakness: Persistent weakness or cramping could signal underactive thyroid levels.
- Swelling: Fluid buildup often shows up as swelling around the eyes, hands, or feet.
For thalassemia patients, the risk of advanced symptoms increases with poor management of iron overload. Timely intervention is critical.
The Role of Subclinical Hypothyroidism
Thalassemia patients are at a higher risk of a condition called subclinical hypothyroidism. This mild form doesn’t always produce obvious symptoms but still puts stress on the body. Regular lab tests to monitor TSH (thyroid-stimulating hormone) levels can help identify it early. Studies suggest that subclinical hypothyroidism is more common than overt hypothyroidism in this population. Learn more about this connection in this study on thyroid disorders in beta-thalassemia.
Overlapping Issues in Thalassemia Patients
The symptoms of hypothyroidism can sometimes mirror or amplify complications already present in thalassemia. For instance:
- Fatigue: Frequently overlaps with anemia symptoms in thalassemia.
- Pale, dry skin: Common in both hypothyroidism and iron overload conditions.
- Difficulty focusing: Could stem from hypothyroidism or chronic low oxygen levels in major thalassemia.
These overlapping issues highlight the need for thorough evaluation and tailored treatment plans. For more insights, check this research on thyroid dysfunction in transfused thalassemia patients.
By learning to recognize these signs and symptoms, especially in the context of thalassemia, patients and caregivers can take proactive steps to maintain overall health and improve quality of life.
Diagnosing Hypothyroidism in Thalassemia
The connection between thalassemia and hypothyroidism might not be obvious at first glance. However, health complications in one area often have ripple effects. Diagnosing hypothyroidism in people with thalassemia requires a detailed approach because the condition can develop silently, often disguised by other symptoms. Let’s explore how medical testing and proactive care can play a key role.
Thyroid Function Tests

Photo by MART PRODUCTION
Thyroid function tests are essential for identifying hypothyroidism, particularly in thalassemia patients who may not show obvious symptoms early on. These tests measure the levels of key hormones in the bloodstream:
- TSH (Thyroid-Stimulating Hormone): High TSH levels are often a red flag for thyroid issues, signaling the gland’s underperformance.
- T3 and T4 (Thyroid Hormones): These provide a deeper look at how well the thyroid is actually functioning.
Regular testing allows doctors to spot abnormalities before significant symptoms develop. Early diagnosis can prevent further complications, especially in individuals already managing a chronic condition like thalassemia. For more insights into thyroid tests, check out this guide on thyroid blood tests.
The Role of Ferritin Levels
Iron overload is a well-documented issue in thalassemia. Frequent blood transfusions can lead to elevated ferritin levels, a marker of excess iron stored in the body. High ferritin not only harms the liver and heart but also directly impacts the thyroid gland. Iron deposits in the thyroid can impair its function, leading to hormone imbalances and, eventually, hypothyroidism.
Monitoring ferritin levels is crucial. It provides indirect but critical clues about the risk of developing thyroid-related problems. Studies suggest that keeping ferritin levels below a certain threshold through iron chelation therapy can reduce hypothyroidism risk. Learn more about the connection between ferritin and hypothyroidism in this study on iron overload and thyroid health.
Importance of Regular Screening
For thalassemia patients, especially those over 10 years old, regular thyroid screening isn’t just beneficial—it’s essential. Hypothyroidism can take years to develop, and symptoms may go unnoticed until significant damage has occurred.
Here’s why periodic testing is so important:
- Prevention: Early screening can catch subclinical hypothyroidism before it progresses to a more severe form.
- Improved Quality of Life: Managing thyroid problems early can reduce fatigue, improve growth in children, and stabilize other bodily functions.
- Tailored Treatment: Regular tests ensure that treatments like iron chelation or hormone replacement are optimized according to the patient’s changing needs.
Routine TSH testing, perhaps annually or biannually, is often recommended for thalassemia patients. Learn more about the guidelines for thyroid dysfunction screening at USPSTF’s recommendations.
Timely diagnosis through these methods can make hypothyroidism in thalassemia manageable and help patients maintain a better quality of life.
Managing Hypothyroidism in Thalassemia Patients
Managing hypothyroidism in people with thalassemia involves addressing underlying iron overload, monitoring hormone levels, and supporting overall health. Here’s how different approaches contribute to better management and improved outcomes:
Iron Chelation Therapy: Its Role in Protecting Thyroid Health
Iron chelation therapy is one of the most critical steps in managing iron overload in patients with thalassemia. This buildup of excess iron can directly harm the thyroid gland, leading to hypothyroidism. Chelation therapy works to remove the excess iron, reducing its damaging effects on organs, including the thyroid.
Several studies have shown that patients on intensive chelation therapy often experience improvements in thyroid function. A reduction in ferritin levels, a key marker of iron overload, has been directly linked to better thyroid health. Chelators like deferoxamine, deferiprone, or deferasirox can effectively minimize thyroid gland damage caused by iron deposits.
For more information, check out this study on thyroid function and iron chelation in thalassemia patients.
Hormonal Replacement Therapy: When is it Needed?
When the thyroid gland cannot produce sufficient hormones, hormonal replacement therapy becomes necessary. Most often, synthetic thyroid hormones like levothyroxine step in to balance thyroid activity. For thalassemia patients, careful attention is given to dosing because their condition may complicate hormone regulation.
Doctors typically monitor the levels of TSH, T3, and T4 hormones to decide when therapy is required. The goal is to restore normal thyroid function and improve symptoms like fatigue, weight gain, or cold sensitivity. Adjustments in medication are often made based on regular thyroid function tests.
Read more about thyroid hormone replacement therapy here.
Nutritional Support: How Diet Can Benefit Thyroid and Overall Health
Diet plays a vital role in supporting thyroid and general health in individuals with hypothyroidism and thalassemia. Key nutrients that affect thyroid function include iodine, selenium, and zinc. A well-balanced diet can improve symptoms and boost energy levels, but it should complement medical treatments rather than replace them.
Foods that may help include:
- Selenium-rich foods like Brazil nuts, tuna, and sunflower seeds, which support healthy thyroid function.
- Iron-absorption blockers (e.g., phytates in certain grains) should be timed carefully around chelation therapy to prevent interference.
- Low-inflammatory foods, such as those in the Mediterranean diet, can help reduce overall metabolic stress.
For guidance on what to eat and avoid, check out this guide to a healthy hypothyroidism diet.
These approaches can provide a comprehensive path to managing hypothyroidism in thalassemia, improving quality of life and long-term health outcomes.
The Importance of Treatment Adherence
Proper treatment adherence is the cornerstone of managing complex conditions like hypothyroidism in thalassemia. Regular medication, doctor visits, and lifestyle changes aren’t just suggestions—they’re lifelines. Skipping doses or ignoring prescribed protocols can derail efforts, leading to a cascade of worsening health issues. Let’s explore why staying on track is non-negotiable and how you can make it easier.
Consequences of Poor Compliance
Failing to follow through with treatments isn’t just a missed opportunity; it’s a risk with real health repercussions. For thalassemia patients managing hypothyroidism, skipping medications or ignoring healthcare recommendations can amplify complications.
- Worsening Symptoms: Hypothyroidism symptoms, like fatigue, cold intolerance, and weight gain, can spiral out of control without consistent treatment. This could severely impact daily function and quality of life.
- Iron Overload Risks: Treating hypothyroidism becomes more challenging when thalassemia-related iron overload isn’t managed. Noncompliance can increase iron buildup, further impairing thyroid function and other organs.
- Long-Term Organ Damage: The thyroid gland isn’t the only organ at risk. Poor treatment adherence can lead to conditions like cardiac complications, liver damage, or growth delays in young patients.
- Higher Healthcare Costs: Missing treatments often results in emergency visits or more intensive interventions later, which are costly and avoidable.
Compliance can mean the difference between managing your condition and letting it manage you. For more insights into the effects of noncompliance in thyroid disorders, explore this study on treatment adherence in hypothyroidism.
Tips for Improving Adherence
Treatment adherence doesn’t have to feel overwhelming. With a few strategic adjustments, staying on track becomes second nature. Here are practical tips to help:

Photo by RDNE Stock project
- Organize Your Medications: Use a pill organizer to keep track of doses for the week. Missing a dose is less likely when everything is in plain view.
- Set Reminders: Alarms on your phone or apps specifically designed for medication tracking can help. Many modern apps even offer detailed tracking for conditions like hypothyroidism.
- Simplify Your Routine: Take medications like levothyroxine at the same time each day, such as right before breakfast, for consistency.
- Engage with Healthcare Providers: Talk openly with your doctor about challenges sticking with treatment. They can modify your regimen or provide alternative solutions that suit your lifestyle.
- Educate Yourself: A little knowledge goes a long way. Knowing why a treatment is crucial makes it easier to prioritize. Learn more tips in this guide from the CDC on medication adherence strategies.
- Make It a Team Effort: Get family members involved. Whether it’s helping track medications or attending appointments, their support can make a big difference.
- Stay Positive: Focus on how consistent adherence is improving your life. Keeping motivation high is key to long-term success.
Improving adherence isn’t about perfection; it’s about progress. Small, deliberate steps make managing hypothyroidism in thalassemia much more achievable. For additional strategies, check out this guide on treatment adherence tips.
Sticking to your treatment plan isn’t just about surviving—it’s about thriving, even with a complex condition like hypothyroidism in thalassemia. Make adherence a part of your daily life, and you’ll notice the difference in your health and well-being.
Long-Term Outlook for Thalassemia Patients with Hypothyroidism
For thalassemia patients, living with hypothyroidism introduces a new layer to their healthcare journey. This combination of conditions requires active management to mitigate long-term effects, but with the right care plan, patients can achieve better health outcomes. Here, we’ll explore how careful monitoring and targeted treatment aim to improve the quality of life and development for those managing both conditions.
Endocrine Monitoring: Emphasize the need for comprehensive checks to manage long-term complications.
Regular endocrine monitoring is not optional for thalassemia patients with hypothyroidism; it’s essential. Iron overload from chronic transfusions doesn’t just affect the thyroid—it puts the entire endocrine system at risk. Over time, other glands, including the pituitary and adrenal glands, may also show signs of damage.
A comprehensive care plan should include periodic screenings of:
- Thyroid-stimulating hormone (TSH) levels – Elevated TSH may signal the thyroid gland is underperforming.
- Ferritin levels – A direct marker for iron overload, which can stress endocrine glands, including the thyroid.
- Growth hormone secretion and markers of puberty – Particularly critical for younger patients with thalassemia.
These tests aren’t only diagnostic; they function as early warnings. Regular monitoring helps spot subtle hormonal changes before they spiral into bigger issues like stunted growth or metabolic disorders. Read more about the importance of endocrine evaluations in thalassemia patients here.
Growth and Development Goals: Share how addressing hypothyroidism can support normal growth and other developmental milestones.
Managing hypothyroidism effectively plays a pivotal role in helping young thalassemia patients reach critical growth and developmental milestones. Untreated thyroid dysfunction can complicate existing challenges like delayed puberty or short stature due to chronic anemia and other endocrine disruptions.
Addressing hypothyroidism should focus on:
- Tailored hormone replacement therapy: Customized doses of levothyroxine or similar medications help normalize T3 and T4 hormone levels, giving younger patients the hormonal support they need for proper development.
- Nutritional strategies: Incorporating adequate iodine, selenium, and zinc supports thyroid hormone production and proper bone development.
- Growth hormone therapies (where appropriate): These are sometimes used alongside thyroid treatments when hypothyroidism directly impacts growth.
When these elements are part of an integrated care plan, children and adolescents with thalassemia and hypothyroidism are more likely to grow taller, enter puberty on time, and enjoy other milestones most take for granted. Comprehensive care not only helps them catch up developmentally but also strengthens their overall resilience.
Learn more about these strategies in this study on growth and endocrinopathies in thalassemia patients.
By ensuring continuous thyroid and endocrine care, thalassemia patients can look forward to improved physical growth and enhanced quality of life—proof that even complex conditions can be managed with the right resources and dedication.
Conclusion
Hypothyroidism in thalassemia presents a complex challenge, deeply intertwined with iron overload and its impact on thyroid health. Regular monitoring and timely intervention are critical to managing this condition effectively. Patients who adhere to iron chelation therapy, undergo annual thyroid function tests, and maintain a healthy lifestyle are more likely to prevent complications.
By staying proactive, thalassemia patients can detect thyroid issues early, improving their overall quality of life. Recognizing the signs, seeking expert care, and following through with treatments can make a significant difference. Empowered with the right knowledge and resources, individuals can take an active role in their health journey.